Healthcare Security
The Numbers Don't Lie—And They're Terrifying
Two healthcare organizations are breached every single day in America. Not hacked. Not "potentially compromised." Actually breached—with patient data stolen, systems locked down, and operations paralyzed.
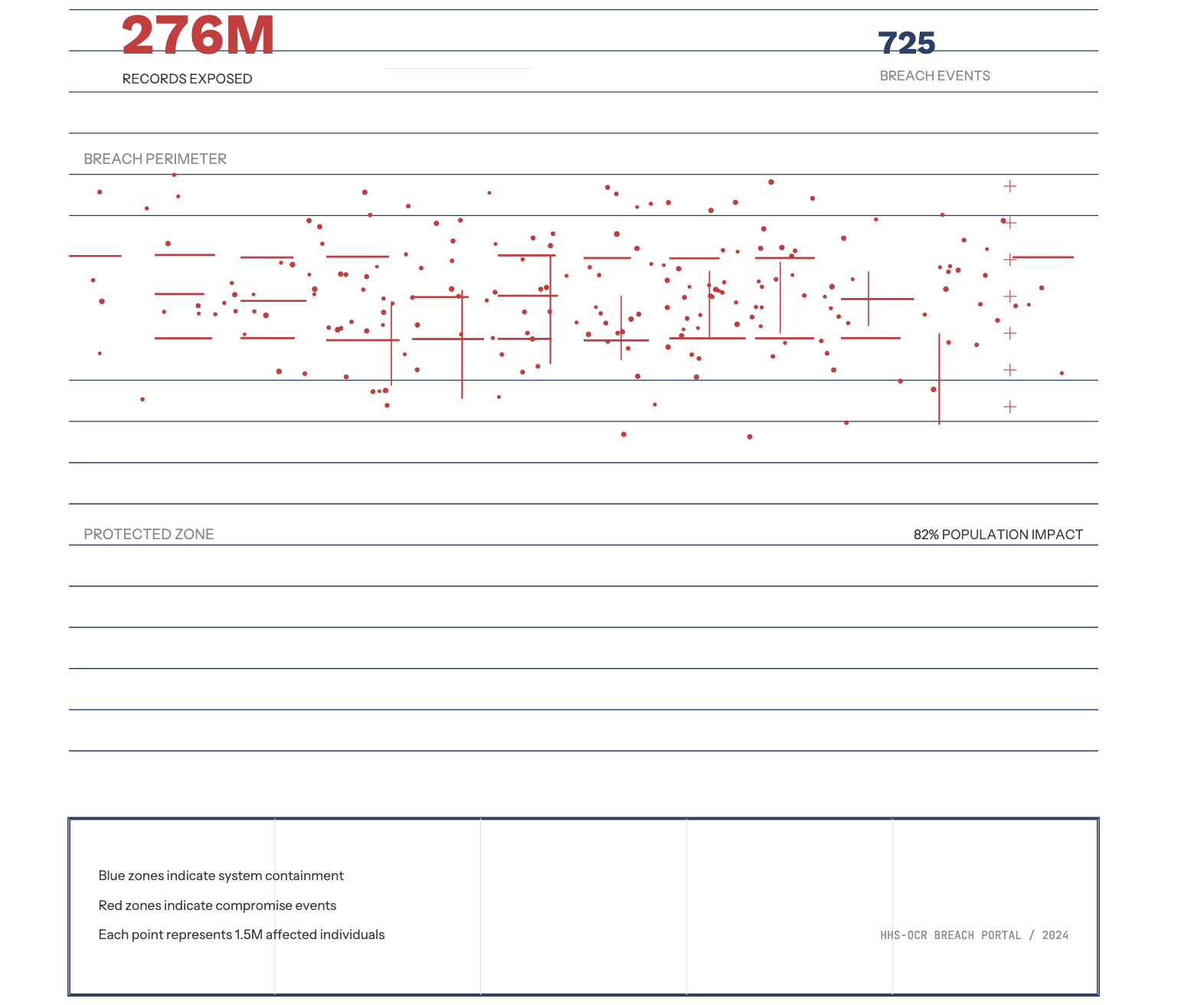
In 2024 alone, 725 large healthcare breaches exposed over276 million patient records—that's 82% of the entire U.S. population. The single largest attack, at Change Healthcare, compromised 190 million records—nearly one in three Americans had their most intimate health information stolen in a single incident.
If you run a small clinic, specialty practice, or mid-sized health system and think "we're too small to be a target,"you're exactly who attackers are counting on.
Why Small and Mid-Sized Organizations Are Prime Targets
Cybercriminals aren't looking for prestige—they're looking for easy money and weak defenses. Your patients' complete medical records sell for $250 to $500 each on the dark web, compared to just $3-5 for a stolen credit card. Why? Because unlike a credit card that can be canceled in minutes,a patient's medical history is permanent. You can't change your cancer diagnosis, reset your blood type, or undo your psychiatric treatment records.
Healthcare suffered more combined ransomware and data theft attacks than any other U.S. critical infrastructure sector in 2024—444reported incidents. And here's the kicker: 81% of these breaches were hacking and IT incidents, meaning they were preventable with proper security controls.
The Real Cost of "Just a Breach"
The average healthcare breach costs $7.42 million—more than any other industry, and healthcare has held this dubious distinction for14 consecutive years. But the financial hit is only the beginning:
It takes an average of 279 days to identify and contain a healthcare breach—the longest of any industry. That's nine months where attackers are in your systems, patient care is disrupted, and trust evaporates.
When ransomware hits, the average demand is $7 million.Change Healthcare paid $22 million—and still ended up with the largest healthcare data breach in history. The company had to provide $9 billion in interest advances to keep healthcare providers solvent after their claims systems froze.
But beyond the ransom, the regulatory consequences are crushing. OCR isn't playing around anymore—in 2024, OCR closed 22 HIPAA investigations with financial penalties, and enforcement activity has accelerated into 2025 with a new focus on risk analysis compliance.
The Ecosystem Problem
Business associates were involved in only one-third of2024's breaches, but those vendor incidents affected 75% of all individuals impacted by healthcare breaches. Your weakest vendor is your greatest vulnerability.
Third-party attacks are skyrocketing because attackers know that small billing companies, lab systems, and tele-health platforms often lack the security resources of major hospital systems—but they have access to the same treasure trove of patient data.
What Actually Works: Security That Protects Care
The healthcare organizations that aren't making headlines are the ones doing these things right:
Know Your Crown Jewels
You can't protect what you don't understand. Map where your most sensitive data lives, who has access, and what would happen if it was compromised tomorrow. This isn't theoretical—attackers begin exfiltrating data before you even know there's a breach.
Treat Vendor Risk Like Patient Safety
Every vendor with access to your network or data is a potential entry point. Demand security attestations, pen test results, and incident response plans. If they can't provide them, they can't access your systems.
Implement Defense in Depth
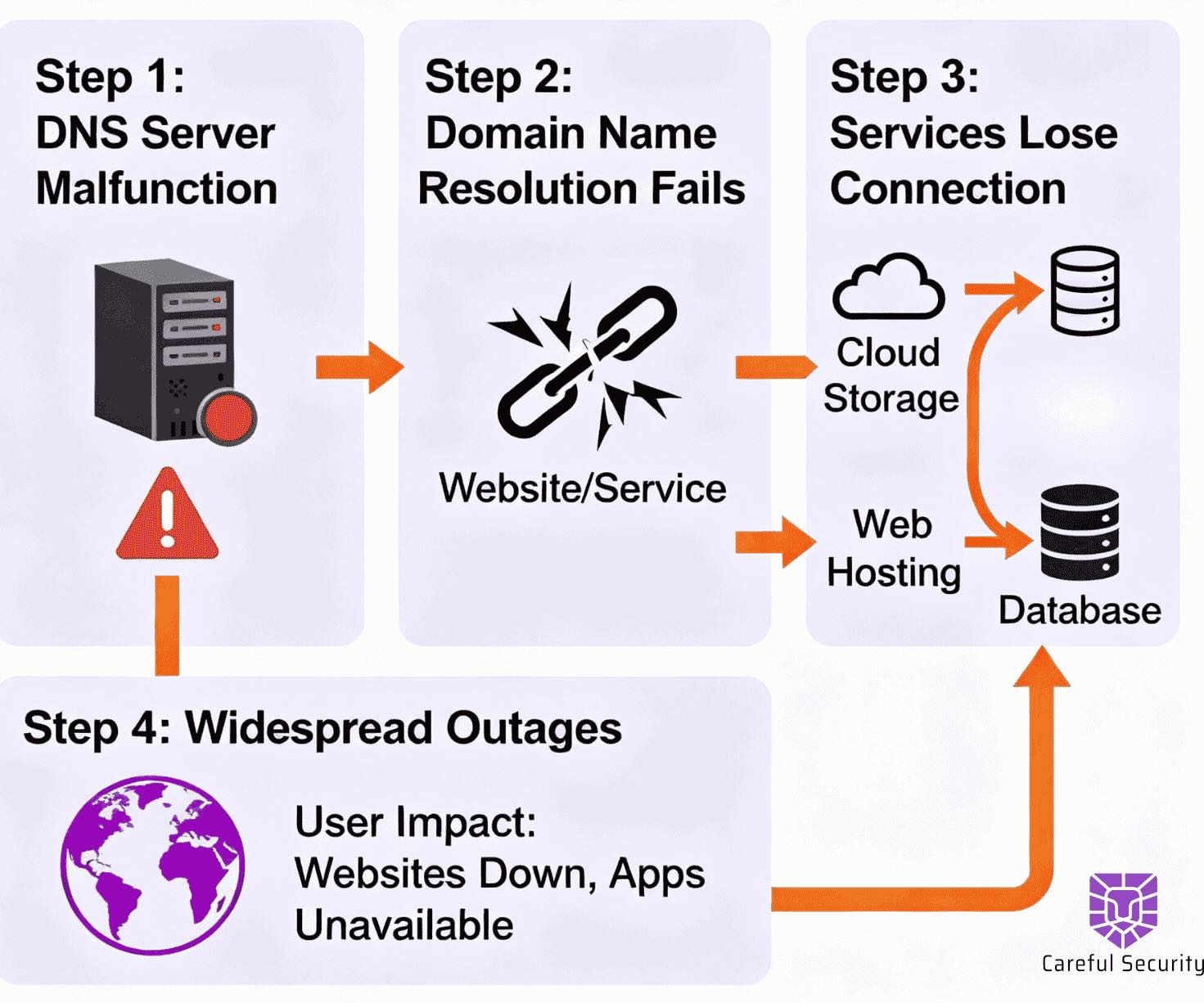
Multi-factor authentication everywhere. Network segmentation. Least privilege access. Phishing is the #1 attack vector,accounting for 16% of all healthcare breaches. Layer your defenses so that when—not if—someone clicks the wrong link, your entire operation doesn't collapse.
Patch Aggressively
Many healthcare organizations still run Windows 7workstations, medical devices with default passwords, and unpatched vulnerabilities. Legacy systems are attractive targets because they're defenseless. If you can't patch it, isolate it. If you can't isolate it,replace it.
Encrypt Everything and Back Up Ruthlessly
Data should be encrypted at rest and in transit. Backups should be immutable, tested regularly, and stored offline. The difference between a contained incident and a catastrophic breach often comes down to whether you can restore systems without paying the ransom.
Drill Your Incident Response
When systems go down at 2 AM, who makes the call to activate downtime procedures? Who contacts OCR? Who handles patient communication? Speed of response determines whether you're down for hours or weeks.
The Bottom Line
Healthcare data breaches aren't slowing down—they're accelerating. Since 2009, over 6,700 large healthcare breaches have exposed 847million individual records. That means nearly every American has had their medical information compromised, many multiple times over.
You hold your patients' most sensitive, permanent, and valuable data. When that trust is broken, it's not forgotten—it's forensically documented in OCR's breach portal, litigated in class action lawsuits, and reported in local news.
Security isn't a luxury, a checkbox, or an IT problem.It's a core component of patient care. Because in healthcare, downtime doesn't just cost money—it delays diagnoses, disrupts treatment, and in the worst cases, causes harm.
The question isn't whether you can afford to invest in security. It's whether you can afford not to.
Cybersecurity Leadership for Your Business
Get started with a free security assessment today.
.avif)
.avif)



.svg)
.svg)
.svg)